Ehlers-Danlos Syndrome (Vascular Type), often referred to as vEDS, is a rare genetic disorder affecting the body’s connective tissues. These tissues provide strength and elasticity to various organs and structures, including blood vessels, skin, and internal organs. vEDS is caused by mutations in the COL3A1 gene, which disrupts the production of type III collagen, a critical component of connective tissue. Early diagnosis and proactive management can significantly improve outcomes and quality of life.
Causes of Ehlers-Danlos Syndrome (Vascular Type)
The primary cause of vEDS is a mutation in the COL3A1 gene. This mutation affects the synthesis of type III collagen, leading to weak connective tissues that are prone to tears or rupture. The condition is typically inherited in an autosomal dominant pattern, meaning a single copy of the mutated gene from either parent is enough to cause the disorder. However, in some cases, vEDS arises from spontaneous mutations with no family history.
Indications of Ehlers-Danlos Syndrome (Vascular Type)
Common indications that may suggest vEDS include:
- Thin, translucent skin with visible veins.
- Easy bruising, even from minor injuries.
- Facial features such as a thin nose, small earlobes, and sunken cheeks.
- Arterial, intestinal, or uterine rupture, which can be life-threatening.
Symptoms of Ehlers-Danlos Syndrome (Vascular Type)
The symptoms of vEDS vary but often include:
- Vascular Symptoms:
- Fragile arteries prone to dissection or rupture.
- Aneurysms.
- Skin Symptoms:
- Thin, translucent skin that bruises easily.
- Delayed wound healing.
- Organ Symptoms:
- Spontaneous rupture of internal organs, such as the intestines or uterus.
Prevention Strategies for Ehlers-Danlos Syndrome (Vascular Type)
While vEDS cannot be prevented, certain measures can help manage risks and prevent complications:
- Regular Monitoring:
- Routine imaging (e.g., MRIs or CT scans) to monitor vascular health.
- Avoid High-Impact Activities:
- Activities like weightlifting or contact sports that increase stress on the vascular system should be avoided.
- Maintain a Healthy Lifestyle:
- Balanced diet and regular, low-impact exercise to support overall health.
- Education and Preparedness:
- Inform family members and caregivers about vEDS.
- Carry a medical alert card or bracelet.
Myths and Facts About Ehlers-Danlos Syndrome (Vascular Type)

- Myth: vEDS only affects blood vessels. Fact: While blood vessels are most impacted, vEDS can also affect skin, organs, and joints.
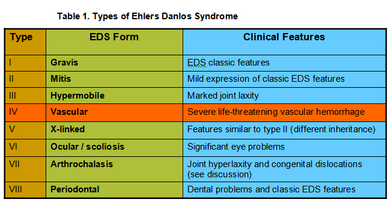
- Myth: All types of Ehlers-Danlos Syndrome are the same. Fact: There are 13 subtypes, each with unique characteristics and challenges.
- Myth: vEDS is always inherited. Fact: In some cases, vEDS results from spontaneous genetic mutations.
- Myth: People with vEDS cannot lead active lives. Fact: With appropriate care, many individuals lead fulfilling lives while managing their condition.
Treatments and Therapy
Medication-Based Treatments
- Beta-blockers: May help reduce stress on blood vessels and lower the risk of rupture.
- Pain management medications: To alleviate chronic pain associated with fragile tissues.
Surgical Treatments
- Surgery is often high-risk but may be necessary for complications like arterial rupture or aneurysm repair. Specialized vascular surgeons are essential for these procedures.
Physical Therapy and Rehabilitation
- Customized programs can improve joint stability and mobility while avoiding excessive strain on fragile tissues.
Lifestyle and Behavioral Interventions
- Engage in low-impact exercises like swimming or walking.
- Avoid smoking and excessive alcohol consumption, which can weaken connective tissues further.
Alternative and Complementary Medicine
- Gentle practices like yoga or tai chi can improve flexibility and mental well-being but should be undertaken cautiously and under supervision.
Psychotherapy and Counseling
- Support for coping with chronic illness and associated anxiety or depression.
- Family counseling to navigate the challenges of managing a genetic condition.
Immunizations and Vaccines
- Staying up-to-date with vaccinations helps prevent infections that could exacerbate complications.
Stem Cell Therapy
- Research into stem cell therapies for connective tissue disorders is ongoing but not yet available for vEDS.
Gene Therapy
- Gene editing technologies like CRISPR show promise for future treatment by targeting the root genetic cause of vEDS.
Top 20 FAQ on Ehlers-Danlos Syndrome (Vascular Type)
1. What is vEDS?
vEDS (Vascular Ehlers-Danlos Syndrome) is a rare genetic disorder that affects connective tissues, with a particular impact on blood vessels, skin, and internal organs. It is the most severe type of Ehlers-Danlos Syndrome.
2. How is vEDS diagnosed?
vEDS is diagnosed through:
- Genetic Testing: Identifying mutations in the COL3A1 gene.
- Clinical Evaluation: Assessing symptoms like thin skin, easy bruising, and arterial complications.
3. Can vEDS be cured?
No, vEDS cannot be cured. However, its symptoms and complications can be managed with proactive medical care, lifestyle adjustments, and regular monitoring.
4. What are the early signs of vEDS?
- Thin, translucent skin that shows underlying veins.
- Easy bruising without significant trauma.
- Fragile blood vessels prone to rupture.
- Arterial, intestinal, or uterine complications.
5. Is vEDS always inherited?
No, while vEDS is usually inherited in an autosomal dominant pattern, some cases arise from spontaneous mutations with no prior family history.
6. How common is vEDS?
vEDS is rare, affecting approximately 1 in 50,000 to 200,000 people worldwide.
7. What activities should be avoided with vEDS?
- High-impact or contact sports.
- Heavy lifting or straining.
- Activities that increase the risk of trauma to blood vessels or internal organs.
8. Can women with vEDS have children?
Yes, women with vEDS can have children, but pregnancy is high-risk. Close monitoring by a multidisciplinary medical team is essential to manage potential complications like uterine rupture or arterial issues.
9. What are the risks of surgery for vEDS?
Surgery in vEDS patients carries increased risks due to tissue fragility, including:
- Difficulty with suturing delicate tissues.
- Increased bleeding risks.
- Post-operative complications.
Specialized surgical teams experienced in managing vEDS are crucial.
10. Can vEDS affect mental health?
Yes, living with vEDS can lead to anxiety, depression, or stress related to managing a chronic condition and its potential complications. Counseling and support groups can help.
11. Are there medications specifically for vEDS?
No specific medications exist for vEDS, but:
- Beta-blockers: May reduce stress on arteries and lower the risk of rupture.
- Pain Management: To address chronic pain.
- Medications are tailored to manage specific symptoms or complications.
12. What are common complications of vEDS?
- Arterial rupture or dissection.
- Spontaneous organ rupture (e.g., intestines, uterus).
- Severe and frequent bruising.
- Joint or skin fragility leading to injuries.
13. Is genetic testing for vEDS widely available?
Yes, genetic testing for vEDS is available and recommended for individuals with suggestive symptoms or a family history of the condition.
14. Can lifestyle changes help with vEDS?
Yes, lifestyle adjustments can reduce risks:
- Low-impact exercises like walking or swimming to maintain fitness without strain.
- A balanced diet to support overall health.
- Avoiding activities that could cause injury.
15. What is the life expectancy for vEDS?
Life expectancy for vEDS varies. Early diagnosis, careful management, and avoiding risky activities can improve outcomes and extend life expectancy significantly.
16. Can children be tested for vEDS?
Yes, children with a family history of vEDS or symptoms like easy bruising or thin skin can undergo genetic testing to confirm the diagnosis.
17. How does vEDS differ from other EDS types?
vEDS specifically targets blood vessels and internal organs, causing life-threatening complications like arterial rupture. Other EDS types typically involve joint hypermobility or skin elasticity without the same vascular risks.
18. What are the most serious symptoms of vEDS?
- Arterial rupture or dissection: Can cause life-threatening internal bleeding.
- Spontaneous organ rupture: Such as the intestines or uterus.
- These require immediate medical attention.
19. Can vEDS be managed without medication?
While medications are often necessary to reduce complications, lifestyle changes, regular monitoring, and avoiding high-risk activities are also critical components of management.
20. What support is available for vEDS patients?
Support includes:
- Genetic Counselors: For family planning and understanding risks.
- Support Groups: Online and local communities for patients and families.
- Specialized Medical Care: From vascular surgeons, cardiologists, and geneticists familiar with vEDS.
Conclusion: Living Resiliently with Ehlers-Danlos Syndrome (Vascular Type)
Ehlers-Danlos Syndrome (Vascular Type) presents unique challenges, but with informed care, individuals can lead meaningful lives. Early diagnosis, proactive management, and access to specialized medical care are key to reducing risks and improving quality of life. By fostering awareness and building supportive networks, we can ensure that those with vEDS receive the care and understanding they need. Advances in research continue to offer hope for better treatments and a brighter future.
Related video: